The New UK Health Secretary's First Official Visit was to a GP surgery. Here’s Why That is Important
Headlines on growing waiting lists, ambulance response times and overcrowded hospitals provide a regular reminder of the challenges that the NHS is facing. Treating those needing care in an NHS hospital is a growing pressure as people wait months and years for necessary care.
In this background, the new Labour Health Secretary’s approach to the NHS may seem strange. Wes Streeting’s official first visit on the job was unusually a GP practice. On this visit, he promised to 'divert billions of pounds from hospitals to GPs'. This approach is no accident. He has previously called for a renewed focus on health outside hospital walls, and the Labour government has signalled support for a 'neighbourhood health service'.
It's not a new concept. The idea that we should be supporting people’s health where they live, and work has been around a while. For the past few decades, the NHS has tried and failed to "shift care and support outside hospital walls".
Why, in a world of struggling hospitals and waiting lists for operations, are we looking outside hospital walls, though?
Solving the hospital crisis is nearly impossible without looking outside hospital walls. One obvious reason is that people don't just get cared for in hospitals. For hospitals to function well, you need to have GP surgeries, community care, and social care organizations sharing the burden with the resources to support our health needs.
That’s not to say our hospitals aren’t vital and need more support. When it comes to staff and capital investment, our hospitals need to be more resourced compared to similar systems.
Yet, we’ve spent decades focusing funding and resources on hospitals, and it hasn’t worked. Hospitals were in crisis well before the pandemic arrived. The idea that many of the solutions to hospital crises lie outside a hospital is a promising approach.
To truly understand why Wes Streeting’s approach is significant, we need to go deeper and understand why health outside hospital walls matters.
The changing nature of our health need
Over the last decade, in the UK, we have been spending more years in ill health. Much of this has been driven by rising chronic illnesses which don’t have “one off cures / treatments”. They also need to be continuously managed throughout life across hospitals, GPs and other care support.
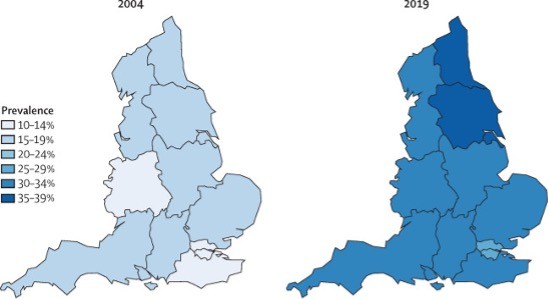
Source: Lancet, O’Flaherty et al, 2021
These illnesses are also shaped by a complex factor but particularly associated with sociodemographic, lifestyles, and environments outside hospital walls. When people don’t have the right support, we end up with a situation like the UK where 2.5 million people are out of work due to long-term sickness.
Add to that an ageing population who need and will increasingly support to be cared for daily, it’s clear we have challenges.
While hospital care is vital and lifesaving, our changing health needs mean we need more support where we live, and work compared to what we get.
The social determinants of health
Out of hospital isn’t just about “healthcare” though. It’s about shifting to look at all public services from a health lens.
There's also a growing body of evidence that suggests it's not just healthcare that matters for our health but wider determinants of health. These wider determinants include warm homes, safe neighbourhoods, jobs where we feel a sense of control, good income and education, air quality, public transport and good social relationships. Also important are things like regulations on fast food outlets, our employer's health and wellbeing policy, and government support for those with low incomes.
A shift in focus to health and healthcare outside hospital walls means a more holistic approach that can consider these factors.
Many studies have found these factors have powerful effects on our lives. Whether its direct effects like pollution exacerbating asthma or long-term indirect effects like lack of social interaction impacting heart health. These factors can work together to have complex impacts. For example, kids in the most deprived parts of the UK are twice as likely to be obese compared to their most affluent counterparts and more likely to have a higher frequency of fast food outlets around them.
A significant issue in the UK is health inequality. People in the most deprived parts of the UK are dying almost a decade earlier than their well-off peers. Here, too, these social determinants seem to play a substantial role.
What's more, there is increasing evidence that multiple biological mechanisms interlink with these social determinants to shape our health. From epigenetic processes (processes that regulate gene expression) to physiological impacts of chronic stressors, our biology doesn't work in isolation from our socio-environmental factors.
This evidence on social determinants isn't without controversy, though. The relationships between health and these determinants represent long, complex causal pathways and bidirectional relationships. Yet, the consistent evidence of strong associations across many of these social determinants and a diverse range of health outcomes in varying settings suggests these are essential forces we should care about in delivering health.
Health workers who support people where they live, and work have deep insights into these social determinants of health. A shift of health services outside hospital walls means a shift in presence of the health system outside hospital walls. Here in the "neighbourhood", we can get rich insights into what matters for people’s health and what we can do about it.
For health workers, local authorities and policymakers, this gives much-needed context on the life circumstances of the people they treat so the right decision can be made for care. This is valuable whether you're receiving hospital care or going to a GP appointment.
This approach means, we can better understand how the NHS might work jointly with other organisations to support people's health needs. This can help us systematically change how public services are organised to support health.
Health is a complex recipe.
Thinking about health outside hospital walls is about more than sharing the burden of healthcare across hospitals, GPs and community and social care. It’s an acknowledgement that our health is made of a complex recipe that includes healthcare, socio-economic circumstances, our environment, behaviours and our biology. Health, cannot just be the responsibility of hospitals alone.
Right now, this is all just a pipe dream. The NHS has repeatedly promised this type of ‘out of hospital’ reform before, but there has yet to be large-scale change. Resources have consistently been redirected from hospital settings to hospitals.
Yet, thinking about "health" outside hospitals is a no-brainer. We must address the nation's growing ill health and changing health needs with a serious focus on it. Here's hoping that Wes Streeting's first official visit suggests something is about to change outside hospital walls for the better.